Introduction: Multiple myeloma (MM) is a disease of the elderly with a median age of 69 years at diagnosis. In addition to advanced age, many of these patients are frail with pre-existing comorbidities and have been historically excluded from clinical trials evaluating chimeric antigen receptor (CAR) T-cell therapy for relapsed refractory (RR) MM. It has been shown that chronologic age alone should not be a barrier towards effective treatment modalities including stem cell transplant and CAR T and that instead of age, frailty scores should be incorporated into CAR T screening and eligibility assessments. As there is limited literature on safety and efficacy of CAR T-cell therapy in frail patients, we conducted a multi-center retrospective study to evaluate clinical characteristics and outcomes of frail patients with RRMM who received standard of care CAR T-cell therapy in real-world practice.
Methods: Three U.S. academic medical centers contributed data which included patients with RRMM who had received idecabtagene vicleucel (ide-cel) between 8/30/2021 and 05/31/2023. Frailty was defined using the simplified frailty index by Facon et al (score based on age + ECOG performance status + comorbidity index; frail = score ≥2). Descriptive statistics were used to analyze clinical characteristics such as age, performance status, and comorbidities. Response outcomes were evaluated using IMWG criteria. Adverse events were graded based on the ASTCT and CTCAE v5.0 criteria. Key data-points included incidence and severity of cytokine release syndrome (CRS), immune effector cell associated neurotoxicity syndrome (ICANS), infections, treatment-related mortality (TRM), overall response rates (ORR), partial response (PR), very good partial response (VGPR), complete response (CR), progression-free survival (PFS), and overall survival (OS).
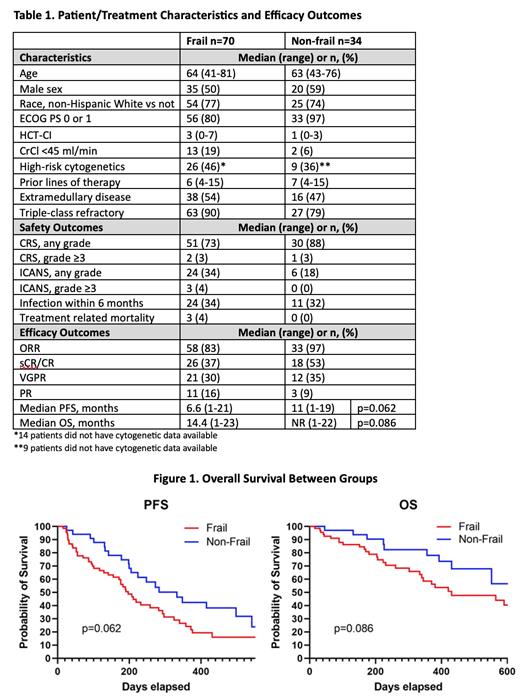
Results: Of the 104 patients analyzed (age range 41-81), 70 (67%) were considered frail at the time of CAR T-cell infusion. The frail group had a high proportion of patients with renal insufficiency (19% vs 6%), high-risk cytogenetics (46% vs 36%), extramedullary disease (54% vs 47%), performance status ≥2 (20% vs 3%), and worse comorbidity index (median 3 vs 1) but were otherwise similar to the non-frail group (Table 1). While patients in the frail group experienced less CRS (73% vs 88%) and more ICANS (34% vs 18%) when compared to the non-frail group, incidence of grade 3+ CRS and ICANS were similar between the two groups. Rates of infection were also similar between the groups with nearly one-third of the patients experiencing an infection within 6 months post CAR T.
With a median follow up of 8 months, best ORR was 83% (37% sCR/CR, 30% VGPR, 16% PR) in the frail group vs 97% (53% sCR/CR, 35% VGPR, 9% PR) in the non-frail group. Median PFS was 6.6 months in the frail group vs 11 months (p=0.062) in non-frail group. Median OS was 14.4 months in the frail group and was not reached (p=0.086) in the non-frail group (Figure 1). TRM was observed in 3 (4%) patients in the frail group. There was no treatment related mortality observed in the non-frail group.
Conclusion: A majority of patients treated with standard of care ide-cel for RRMM in this real-world experience were frail by simplified frailty index. While these patients had worse performance status and higher comorbidity burden at the time of CAR T infusion, they did not experience any excessive high-grade toxicities including TRM. When compared to the non-frail group, frail patients had numerically inferior but statistically similar depth and duration of response. This study supports the tolerable safety and reasonable efficacy of CAR T-cell therapy for frail MM patients in a real-world practice and highlights the need to study outcomes in this patient population in larger registry-based data as well as clinical trials.
Disclosures
Ahmed:Kite, a Gilead company: Research Funding; Bristol Myers Squibb: Consultancy. McGuirk:Pluristem Therapeutics: Research Funding; Gamida Cell: Research Funding; Bellicum Pharmaceuticals: Research Funding; Kite: Consultancy, Research Funding; Astellas Pharma: Research Funding; Fresenius Biotech: Research Funding; Novartis: Research Funding; EcoR1 Capital: Consultancy; Magenta Therapeutics: Consultancy; Allovir: Consultancy, Research Funding; Juno Therapeutics: Consultancy. Khouri:Janssen: Consultancy, Honoraria; GPCR Therapeutics: Honoraria. Valent:Alexion, AstraZeneca Rare Disease: Research Funding. Hashmi:Jannsen: Honoraria, Speakers Bureau; BMS: Honoraria; Karyopharm: Speakers Bureau; Sanofi: Honoraria, Speakers Bureau; GSK: Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal